Prostatitis (inflammation of the prostate) is one of the most common diseases of the genitourinary and reproductive system in men today. This is a pathological condition that can combine inflammation of the prostate gland itself and the area around it. There are several types of this disease, each of which has different symptoms.

Some men with this disease may experience severe pain, while others will not be bothered by the disease; For others, prostatitis symptoms appear periodically and are chronic. However, the symptoms of the disease significantly impair a person's quality of life.
reason
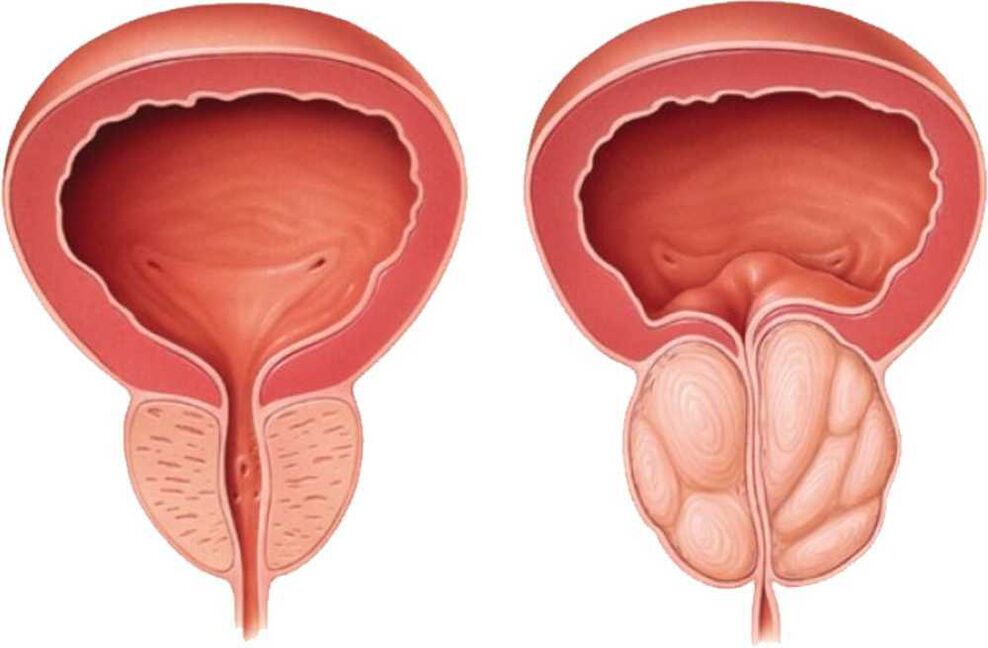
The prostate is a walnut-shaped gland that is part of the male reproductive system. The main function of the prostate is to produce fluid, which is responsible for the quality of sperm. The gland surrounds the urethra at the bladder neck and prevents sperm from returning to the bladder. It, like a natural valve, separates two systems - the urinary and reproductive systems. This organ holds urine in the bladder and lets it out when needed. Inflammation of the prostate negatively affects both the reproductive function of a man and the state of his urinary tract.
Acute bacterial prostatitis is the least common but mildest type of prostatitis known. It is usually caused by a sudden outbreak due to a bacterial infection. It is easily diagnosed as there are a number of characteristic symptoms and signs. This severe urinary tract infection is most often accompanied by high fever and chills and in this case an immediate visit to the doctor or hospital will be required. Men of all ages are susceptible to this disease, especially those with weakened immune systems. Symptoms of this form of prostate disease include painful urination; difficulty or inability to completely empty the bladder, cramping pain in the lower abdomen, perineum, back or pelvis; chills and fever.
The chronic bacterial form of prostatitis is similar in its symptoms to the acute bacterial form, but develops gradually and its symptoms are less serious. It is characterized by repeated infections of the urinary tract in men; this inflammation occurs in representatives of different age groups, but is more common in young people and men of reproductive age.
Chronic non-bacterial prostatitis (chronic pelvic pain syndrome, non-bacterial prostatitis, prostatodynia), the most common type of the disease. The exact causes of this type of inflammation are not known. However, the disease can begin with an acute or low-grade chronic infection, followed by inflammation, or provoked by muscle spasm in the pelvic area.
In this case, inflammation in the prostate can occur without any symptoms, or the symptoms can be hidden. Sometimes patients experience pain in the genitals, discomfort in the pelvic area, difficulty or pain during urination, and sometimes pain during or after ejaculation.
Asymptomatic prostatitis is also common. The diagnosis is established only when the patient presents for another disease and the main complaints are related to symptoms that are not associated with prostatitis. In such cases, it is confirmed by tissue biopsy or urine and sperm analysis.
What causes prostatitis?
The immediate causes of prostatitis are not clearly defined by the medical community. However, there are several accepted theories. In the most studied cases, the inflammatory process in the prostate is clearly related to acute or chronic bacterial infections. They enter the prostate through the urethra. Bacterial prostatitis is not contagious and cannot be sexually transmitted. A sexual partner cannot "catch" this infection.
Certain specific conditions or medical procedures related to diagnosis or treatment increase the risk of bacterial prostatitis. There is a good chance that the person has had a catheter or other instrument inserted into the urethra because of treatment for a urinary tract infection or bladder infection.
Prostatitis can be caused by atypical microorganisms, such as chlamydia, mycoplasma (transmitted through sexual contact) and ureaplasma. It can also be caused by a chemical or immunological reaction to an initial injury or infection. Muscle spasms in the pelvic area can cause pain in the prostate area. It can also be a response to infection or inflammation of the prostate gland.
Doctor's opinion:
Prostatitis is an inflammatory disease of the prostate that can lead to various unpleasant symptoms, such as pain in the genitourinary system, urinary problems and general malaise. Doctors recommend seeking help at the first signs of the disease, as irrational treatment or its lack can lead to chronic prostatitis and complications. To make an accurate diagnosis and determine the optimal treatment, you should contact a urologist who will perform the necessary examinations and choose the appropriate therapy. It is important to remember that prostatitis requires a comprehensive approach to treatment, including drug therapy, physical therapy and regular monitoring by a specialist.
Prostatitis. How to quickly cure inflammation of the prostate.
Symptoms
Symptoms depend on the type of prostatitis and the type of infection that caused it. Often patients do not notice any signs of the disease, while some experience symptoms similar to urinary tract infections. Please note that other diseases can cause the same or similar symptoms. It is very important that a diagnosis is made by a medical professional to determine if the patient really has prostatitis and what type it is.
In acute bacterial prostatitis, the symptoms are severe and require immediate emergency medical attention. Common ones are: chills, fever, burning during urination, heaviness in the lower abdomen, inability to empty the bladder.
In chronic bacterial prostatitis, symptoms are similar to acute bacterial prostatitis infections, but there is no fever. Other symptoms: burning during urination; frequent urge to urinate, especially at night; pain in the perineum, testicles, bladder and pain in the lower back; pain during ejaculation. Symptoms may be episodic, with flares and remissions. The started process turns into calculous prostatitis.
Symptoms of nonbacterial prostatitis (chronic pelvic pain syndrome) include difficulty and sometimes painful urination, discomfort or pain in the perineal area, bladder, testicles, and penis, and difficult or painful ejaculation. Sometimes, or even more often, these symptoms can be indistinguishable from those described above for chronic bacterial prostatitis.
Diagnosis of prostatitis
Correct diagnosis is very important for the treatment of any disease and especially for prostatitis. Because the treatment of its various forms does not only vary in duration, but also in the range of methods and tools. In addition, it is extremely important to distinguish the symptoms from other similar ones, such as urethritis, cystitis, prostate enlargement, adenoma or cancer. To make the most accurate diagnosis, you will need several types of tests and studies.
One of the tools that doctors use in diagnosis is the study of symptoms using a special questionnaire that is filled out by the patient. In addition to completing the questionnaire, your doctor may order a physical examination.
To check the state of the prostate gland, the doctor will perform a digital rectal examination. This is a simple examination in which a specialist inserts a lubricated (gloved) finger into the patient's rectum. The prostate is located just in front of the rectum and just below the bladder; palpation allows the doctor to easily detect and examine the problem organ.
In this way the doctor can determine if the prostate gland is enlarged. Irregularities may indicate the presence of prostate cancer. The specialist will also be able to assess the degree of pain or discomfort the patient experiences when the doctor presses the muscles and ligaments of the pelvic floor and perineum. If the patient does have prostatitis, this manipulation may cause immediate pain or discomfort, but it also does not cause significant long-term destruction or pain.
If the doctor requires a more accurate diagnosis or decides that a biopsy is necessary, he can order a transrectal ultrasound, which allows him to visualize the prostate gland.
If a specialist suspects you have prostatitis or another prostate disease, they may refer you to a urologist, a doctor who specializes in diseases of the urinary tract and male reproductive system, to confirm the diagnosis.
The urologist will repeat some of the tests and may analyze different urine samples as well as samples of prostate fluid obtained by massaging the prostate during rectal palpation. Samples of urine and prostate secretions are examined for signs of inflammation and infection. These tests will help your urologist diagnose your problem more accurately: if there is inflammation or infection in the urethra, bladder or prostate gland.
Some doctors may order blood and sperm tests to look for abnormal microorganisms, white blood cell counts, or other signs of infection.
A urologist may order a cystoscopy, in which a small special telescope is inserted through the urethra and the bladder, urethra, and prostate are examined. The urologist can also order urine flow tests, which help measure the intensity of the flow and the presence of obstructions caused by inflammation of the prostate gland, urethra or spasm of the pelvic muscles.
Interesting facts
- Prostatitis can affect men of any age: Although it is more common in men over the age of 50, even younger men can develop prostatitis.
- There are many causes of prostatitis:The most common causes include bacterial infections, inflammation and blocked prostate ducts. In some cases, the cause may be unknown.
- Prostatitis can have a number of symptoms:These can range from mild discomfort during urination to severe pain, fever and chills. Symptoms often depend on the type of prostatitis and its severity.
Other people's experiences
Prostatitis is a common disease in men that causes inflammation of the prostate gland. People who face this problem note that the symptoms of prostatitis can be quite unpleasant and interfere with normal life. Many people express concern about pain in the perineum, urinary problems and general discomfort. However, it is important to remember that prostatitis is a reversible disease, and timely consultation with a doctor, appropriate treatment and lifestyle changes can help cope with it. People are advised not to delay the visit to the specialist and follow the recommendations for a quick recovery.
Treatment
Treatment of prostatitis directly depends on the type of bacterial infection that was diagnosed during the study.
For acute bacterial prostatitis, the patient will need to take antibiotics for at least 14 days. Sometimes patients require hospital treatment and intravenous antibiotics. If the patient has difficulty urinating, a catheter will be needed. If the disease does not respond to treatment, the doctor prescribes other antibiotics and the course continues until complete recovery.
It is important to know that when taking antibiotics you should always follow your doctor's instructions. Don't miss another appointment or stop treatment early just because you think your symptoms are gone.
If chronic bacterial prostatitis is diagnosed, you will need to take antibiotics for a longer period than in the acute form. About 75 percent of all cases of chronic bacterial prostatitis heal completely within 6-7 months. Sometimes symptoms return and antibiotic therapy must be repeated over and over again. In cases that do not respond to this treatment, long-term low-dose antibiotic therapy is recommended to relieve symptoms. In some rare cases, surgery may be necessary if the patient has specific anatomical problems, such assh. scar tissue in the urethra, which interferes with prostate treatment.
The patient may not need antibiotics if diagnosed with chronic pelvic pain syndrome. Urologists often encounter difficulties when trying to decide whether a patient has bacterial or non-bacterial prostatitis. Sometimes previous antibacterial therapy hides the diagnosis. In such cases, antibiotics may be prescribed, at least initially, even when a definitive diagnosis of bacterial prostatitis has not been established. Your response to antibiotic therapy will determine whether it should be continued.
Many patients without an actual infection may feel better during antibiotic treatment, because most antibiotics have a direct anti-inflammatory effect.
Depending on the symptoms and dynamics of treatment, patients can be prescribed several methods to quickly restore health. Some specialists prescribe alpha blockers in addition to antibiotics. These medications help relieve spasm and relax the muscles around the prostate and the base of the bladder, eliminating pain during urination. Folk remedies are often used successfully - anti-inflammatory herbal preparations, analgesic infusions, muscle relaxants, herbal extracts (quercetin and/or bee pollen). Prostate massages will release fluids that are causing pressure and pain in the prostate.
Hot baths, mud baths, or other various heat treatments (applying local heat in the form of a hot water bottle or a heating pad) will provide relief and temporarily relieve the discomfort associated with the infection. If sitting becomes very uncomfortable, patients are advised to use a special pillow.
Acupuncture, reflexology and relaxation exercises in addition to primary treatment can also help relieve some symptoms. You may be advised to follow a special diet, avoid certain foods (such as spices) and drinks (such as caffeinated drinks, acidic drinks) and avoid triggers (such as cycling) that can make the pain worse. prostate.
Only preventive measures, timely diagnosis and an integrated approach to the treatment of the prostate gland will preserve men's health for many years. Take care of your second heart - the prostate!
Frequently asked questions
How can I tell if I have prostatitis?
Pain, burning during urination Difficulty urinating Leakage of urine Frequent urination Cloudy urine Blood in the urine (hematuria) Pain in the abdomen, groin, suprapubic area General malaise symptoms (fever, weakness)
What is prostatitis and why is it dangerous?
Prostatitis is an inflammatory process in the prostate gland. The main threat of such an inflammatory process is that it may not appear for a long time. Sometimes a man can be sick for several years and not even realize that he needs treatment.
Why does prostatitis occur in men?
Causes of prostatitis Its symptoms usually appear in men aged 30-50 years. Most often, the cause is an infectious lesion due to the penetration of pathogenic flora from the urogenital canal or the glands of the genitourinary system. This is explained by the proximity of the urethra and the anus.
How do you get prostatitis?
Bacteria that enter the prostate gland through the urethra, blood circulation, lymph, Disorders of the rhythm of sexual life, reduced immunity, Sexually transmitted infections (gonorrhea, trichomoniasis, chlamydia, etc. ), damage to pelvic organs and tissues.
Useful tips
Tip #1
Signs of prostatitis can be different, including pain in the perineum, frequent urination and increased body temperature. At the first suspicion of prostatitis, be sure to consult a urologist for diagnosis and treatment.
Tip #2
Look at your lifestyle: lead an active lifestyle, drink more water, give up bad habits, include more fruits and vegetables in your diet. This will help strengthen the immune system and prevent the development of prostatitis.
Tip #3
Regularly perform preventive examinations with a urologist, even if there are no obvious symptoms of the disease. Early detection of prostatitis will allow you to start treatment at an early stage and avoid complications.























